Did you know epilepsy is common?
Approximately 1% of the U.S. population will experience an epileptic seizure during life.
November is National Epilepsy Awareness Month. Here are some key facts and treatments for epilepsy from a Mayo Clinic doctor.
- Diagnosis: Epilepsy is diagnosed when a person is found to have a predisposition for recurrent unprovoked seizures.
- Treatment: Many individuals respond well to anti-seizure medications. But a third of people with epilepsy have drug-resistant epilepsy, meaning that seizures recur despite appropriate treatment with anti-seizure medications. Neurostimulation can be a valuable treatment option when medications fail to control seizures.
- Impact: Epilepsy can be a challenging condition for individuals and family members. Recurrent unpredictable seizures can have a major impact on a person’s safety, independence, sense of security and quality of life.
Treatment beyond medications with neurostimulation
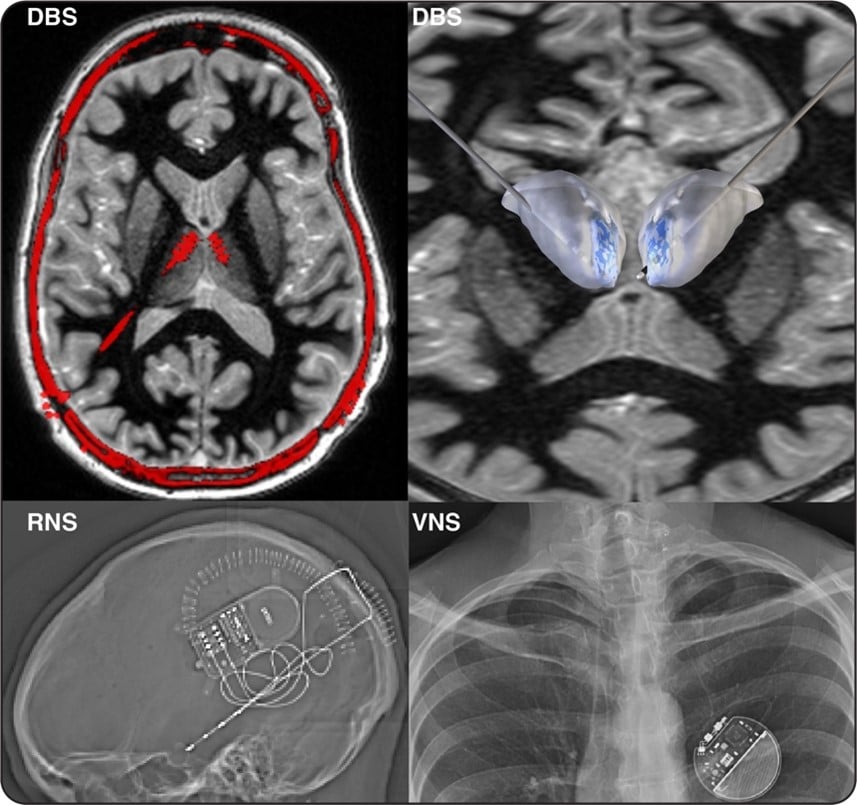
There are three Food and Drug Administration (FDA)-approved neurostimulation approaches for the treatment of drug-resistant epilepsy:
- Deep brain stimulation (DBS).
- Responsive neurostimulation (RNS).
- Vagus nerve stimulation (VNS).
All of these approaches use a stimulator unit and a set of electrodes placed under the skin to deliver stimulation therapy to reduce seizure frequency. Each has been rigorously studied and has been shown to produce a significant reduction in the frequency of seizures for many patients.
It’s important to find the right approach for each individual. Research efforts to improve the personalization of neurostimulation are ongoing. Talk to your health care provider to identify the best treatment option for you.
What makes each approach unique?
- Deep brain stimulation (DBS) uses two electrodes placed on each side of the brain into a deep structure called the thalamus. The electrodes are connected to a stimulator unit placed in the chest. The thalamus is a relay center with widespread connections to other brain regions. So the precise location of seizure onset may not be needed for DBS. The average patient will have about a 50% reduction in seizure frequency after the first year, which increases to 75% after 5 to 10years. Over the past several years the epilepsy research community has worked to identify the optimal targetof DBS electrodes, and to identify individuals who are likely to respond well to DBS therapy.
- Responsive neurostimulation (RNS)uses two electrodes that are placed into one or two brain areas of seizure onset. The electrodes are connected to a stimulator unit placed in the skull. The RNS system detects brain activity and delivers stimulation in response to changes in brain activity. The RNS system also can identify electrographic seizure activity for some individuals, which can help guide ongoing clinical care. The one-year and 5-to-10-year performance of the RNS system is similar to DBS. Precise information about the brain region of seizure onset is needed to guide electrode placement. The RNS system is unique in its ability to provide detailed brain recordings that mayassist clinical decision-making.
- Vagus nerve stimulation (VNS) uses electrodes placed around the vagus nerve in the neck that areconnected to a stimulator placed under the skin in the chest. VNS placement does not require brain surgery, unlike DBS and RNS. Precise seizure onset location is not needed for the use of VNS, which is similar toDBS. The average patient should expect a reduction in seizure frequency of about 30% to 40% after the first year. VNS is FDA approved for adults and children 4 years of age and older. In contrast, DBS and RNS are approved for adults 18 years of age and older. A multicenter study is underway to evaluate the use of RNS in children with epilepsy.
Neurostimulation is a rapidly evolving area for the treatment of epilepsy. It is important to work with an experienced team who can stay up to date with advances in the field, evaluate your epilepsy condition in detail, facilitate a thorough discussion of treatment options, and identify the best treatment option for you.
Learn more about how Mayo Clinic’s epilepsy experts can help manage your epilepsy at MayoClinic.org/epilepsy.
__
Nicholas M. Gregg, M.D., is an adult neurologist and epileptologist at Mayo Clinic in Rochester, Minnesota, who specializes in neurostimulation treatments for epilepsy, including deep brain stimulation, responsive neurostimulation and vagus nerve stimulation. His research is focused on personalized neurostimulation for the treatment of drug-resistant epilepsy, as well as seizure risk forecasting so that interventions can be taken to prevent seizures or reduce seizure risk. Dr. Gregg works with scientists and engineers to transform epilepsy care, and is active in mentoring graduate students and medical trainees.
